Sightsync x Roche
Designing Inclusive Learning for AMD Patients and Caregivers
Role: UX Lead
Timeframe: 3 Months
Overview
The app is designed primarily for AMD patients and their caregivers—to guide and support them through accessible learning, and to enable collaboration in compiling, storing, and sharing health data throughout their journey. This specific focus on AMD and education makes it the first app of its kind—funded by Roche and currently in development.
As the lead designer, I worked across nearly every part of the app experience and oversaw the full design process—but here’s a closer look at the learning platform, which formed the heart of the user journey.

Top Level Goals
Design an accessible audio learning experience
For both AMD patients and caregivers—one that delivers timely, relevant content and helps people feel informed, supported, and connected.
Drive & Track Engagement
Encourage consistent engagement during the clinical trial by designing for habit-building and tracking usage. We’ll monitor engagement data throughout, aiming for at least 70% of users to interact with the app 3× per week.
Deliverables to Roche
Deliver high-quality, on-brief outputs to Roche—ensuring all research, design, and content deliverables align with clinical goals, timelines, and partner expectations.
Competitive Analysis
Since no directly comparable apps existed for AMD-specific learning, I broadened my research to adjacent fields—focusing on audio-first products, storytelling platforms, and e-learning tools designed for older adults and people with visual impairments.
I created detailed competitive profiles evaluating factors like marketing strategy, target audience, core features, usability, layout, navigation, content, and accessibility. To deepen the analysis, I also conducted a SWOT assessment to understand strengths, weaknesses, opportunities, and gaps across the landscape.
Opportunities and Challenges
Opportunity #1
Deliver stage-specific content through meaningful onboarding
With 300 participants in the clinical trial, we have a rare opportunity to individually onboard users and assign them to learning paths that match their stage—newly diagnosed, long-term management, or caregiving. This allows us to set expectations, deliver relevant information, and build trust early. Well-timed, personalized content increases clarity and supports better decision-making throughout the AMD journey.
Opportunity #2
Foster emotional connection through storytelling and shared voices
Hearing from others with similar experiences helps users feel seen and supported. By featuring recurring speakers and personal stories, we build trust, comfort, and a sense of belonging. This emotional layer encourages return visits and creates a human, empathetic experience. In future iterations, interactive elements could deepen that sense of connection even more.
Opportunity #3
Ensure low-barrier access through audio-first design
As AMD progresses, users may lose access not only to text-based platforms or social tools, but also to essential information—like pamphlets about their diagnosis or treatment. Audio remains one of the few formats that’s still usable, familiar, and low-effort. By delivering clear, screen-free content, we help users stay informed, independent, and engaged throughout their journey.
Challenge #1
Low digital adoption among older adults with vision loss
This age group is not typically made up of early adopters—and many are hesitant to engage with new digital tools, even without accessibility barriers. When combined with the emotional and functional impact of vision loss, adoption becomes an even greater challenge. To succeed, the app must feel approachable, non-technical, and confidence-building from the very first interaction.
Challenge #2
Designing for emotional and cognitive variability—including caregiver dynamics
Users arrive in very different emotional and cognitive states—some anxious, some disengaged, some navigating care roles for others. Many feel overwhelmed by their diagnosis, burned out from caregiving, or exhausted by medical information that’s hard to understand. Our challenge is to design content and flows that are attuned to these differences—offering the right tone, timing, and flexibility to meet both patients and caregivers where they are.
Challenge #3
Sustaining engagement throughout the clinical trial
In order to prove the platform’s value and secure future funding, we must demonstrate strong user engagement during the trial—not just after. This means keeping participants consistently active, curious, and emotionally connected across the entire testing period. If engagement drops, we risk losing both insight and momentum. The app must offer ongoing relevance, ease of access, and emotional motivation to keep people returning.
Interviews
Using a design thinking approach grounded in accessibility and inclusive education, I conducted interviews with 7 people living with Age-related Macular Degeneration (AMD) as well as their caregivers—ranging from early to late stages of vision loss.
To deepen the research, I also reached out to Retina Suisse, a national advocacy organization, to better understand the broader support landscape and identify gaps in patient education and communication.
These conversations revealed not only the daily challenges of navigating vision loss, but also emotional needs and learning preferences that informed the structure, tone, and features of the app experience.
A few excerpts from my script:
Can you tell me a bit about your (or your loved one’s) experience with AMD so far?
→ Explorative inquiry into their personal story, where they are in their journey.
How did you first get information or support after the diagnosis? What helped—and what didn’t?
→ Check pain points, trusted sources, and gaps in the system.
What kinds of tools or resources do you currently use to manage AMD or support someone with it?
→ Uncovers habits, workarounds, or devices already in use.
What’s the most frustrating or overwhelming part of navigating this condition day-to-day?
→ Highlights opportunity areas and emotional drivers.
Findings from User Interviews
Interview Insight #1
Diagnosis almost always comes with confusion and emotional overwhelm.
Participants shared that their initial diagnosis left them with more questions than answers.
“They handed me a leaflet and said ‘see you in six months’—I didn’t even know what questions to ask.”
Interview Insight #2
People want clear, non-technical explanations.
Interview subjects spoke about how medical terminology often created fear or confusion. Participants preferred clear, friendly information that they were able to pass on in their own words.
“Everything I found online felt too clinical or too scary. I just needed someone to talk to me like a human.”
Interview Insight #3
Caregivers need support too—but are rarely included.
Several caregivers expressed frustration about being left out of the conversation and overwhelmed with the learning curve. Many are also struggling to keep up with medical records.
“We’re navigating this too—with zero guidance.”
Interview Insight #4
Most people make up their own workarounds.
Participants rely on magnifiers, phone settings, and help from family to adapt digitally. Many also modify their living space over time.
“My granddaughter set my phone to dark mode and bigger text. Otherwise, I’d be lost.”
Interview Insight #5
Loss of independence is a common emotional trigger.
The fear of becoming dependent—more than the vision loss itself—came up repeatedly in interviews.
“It’s not the blindness that scares me—it’s becoming a burden.”
Interview Insight #6
Peer stories and shared experiences build trust and hope.
Hearing from others with AMD was described as both comforting and empowering.
“Hearing others' stories in group meetings, makes me know I'm not alone - I can also learn a lot”
Interview Insight #7
First impressions shape trust in tools and information.
The tone and accessibility of a product’s first touchpoint can make or break engagement.
“When I first Googled it, I closed the tab after two minutes. It felt like falling into a black hole.”
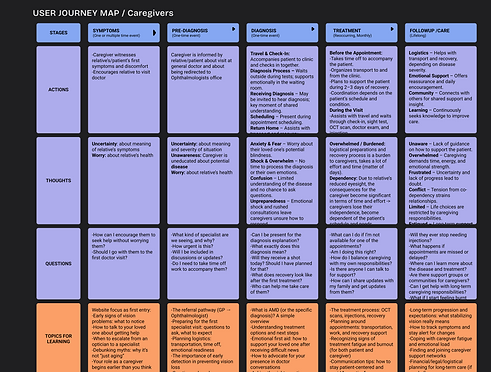
Mapping out the journey was essential for us—it revealed so many small but meaningful nuances. By closely examining each step, I could really see the waiting, the uncertainty, and the anxiety that patients and caregivers experience.
Understanding the medical procedure itself—how much of it involves waiting, brief interactions, and back-and-forth—gave us a new level of empathy. Having this full picture wasn’t just helpful for design; it was huge for aligning the whole team around the real human experience.

Accessibility Needs

AMD primarily affects the macula, the part of the retina responsible for sharp central vision. Users often experience a blurred or dark spot in the center of their visual field. To adapt, they rely on peripheral (edge) vision, which is less precise but still functional.
On top of that, we recognized that older users are often late adopters of technology and less likely to use screen readers—especially since many still have one unaffected eye or varying degrees of usable vision.
Instead of assuming full reliance on assistive tech, we focused on built-in visual flexibility:
-
Large, high-contrast text
-
Adjustable zoom
-
Both vertical and horizontal scrolling
-
A layout that avoids central focus, with main actions placed along the edges
User Testing
We tested with people aged 60+ who had AMD, visual impairments, or used simulation glasses. I recruited participants from the AMD community and my own network, creating a space to learn together.
I used a structured script to stay consistent and reduce bias, while still allowing for open insights.
These sessions gave us crucial input on how vision levels and tech familiarity shaped interaction—directly influencing the MVP’s accessibility and layout.


Next Steps: Development & Clinical Trial
So far, we’ve had limited access to the development team, but we’ve used every moment together to build a strong foundation and game plan. Over the next five months, we’ll collaborate more closely, combining technical development with ongoing research and innovation to bring the app to life. In parallel, I’ll be working with a teammate to scope out stories and record them in multiple languages at my home studio—ensuring the content is as accessible and meaningful as the experience itself.
All the while, another team member will be leading recruitment efforts as we begin our first clinical trial. Throughout this process, we’ll have rich access to users and their stories, gain real-time feedback on how the app works, and collect invaluable insights into how it can best serve people living with AMD.


What I Learned & Implemented
I knew that search is necessary, but typing isn't always ideal—especially for users with low vision or motor challenges. After speaking with our developers, we implemented speech-to-text search, which not only supports accessibility but can also be reused in other parts of the app. A great example of one feature solving multiple needs.
During testing, we read podcast content aloud since real recordings weren't yet ready. This helped me get a strong sense of pacing and tone, and led to the next challenge: finding real speakers—either people sharing their own stories or voice actors narrating others'.